Fetal Anemia

CLINICAL HISTORY – Part I
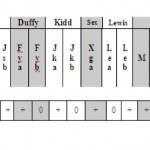
A 26-year-old gravida-4, para-1, woman came for evaluation for fetal anemia. She had one living born child, and 3 consecutive pregnancies ended with intrauterine fetal demise. This is her 4th pregnancy. During her third pregnancy a year ago, antibody screening was positive. RhIg was administered during the fourth pregnancy. Table 1 shows patient ABO/RH forward, back typing and antibody screening panel.
Quiz-summary
0 of 3 questions completed
Questions:
- 1
- 2
- 3
Information
BEGIN QUIZ 1/2 (Please complete Quiz 1 before proceeding to Quiz 2):
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading...
You must sign in or sign up to start the quiz.
You have to finish following quiz, to start this quiz:
Results
0 of 3 questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 points, (0)
| Average score |
|
| Your score |
|
Categories
- Not categorized 0%
-
Click ‘VIEW QUESTIONS‘ for the discussion.
- 1
- 2
- 3
- Answered
- Review
-
Question 1 of 3
1. Question
What antibodies do you identify from the panel?
CorrectThe patient’s serum on panel 1 showed she is group A-, with anti-D and anti-C.
Anti-D Discussion
After the ABO system, the Rh system is the most important blood group system in transfusion medicine with D being the most immunogenic Rh antigen. The original ‘Rh’ antigen stimulated a transfusion reaction, which was investigated by Levine and Stetson in 1939. The reactions of this antibody paralleled those of the anti-’Rh’ reported by Landsteiner and Wiener in 1940 but stimulated in animals. Years later, upon recognition that the human and the animal anti-’Rh’ did not react with the same antigen, the antigen name switched to D and the system took the Rh name. Testing for the D antigen is included as part of routine donor and patient typing with “Rh positive” and “Rh negative” referring to the presence or absence of the D antigen on red blood cells. The D antigen is distinguished from other blood group antigens in that it is composed of at least 30 epitopes distributed along the extracellular portions of the RhD protein.
Most anti-D is IgG with some IgM and can cause a mild to severe, immediate/delayed transfusion reaction. Anti-D can also cause mild to severe hemolytic disease of the fetus and newborn (HDFN). The optimal technique for detection is the indirect antiglobulin test (IAT). Saline IAT is used in this case to identify IgM anti-D, confirming , rule out Rh-Ig.Anti-C Discussion
The C antigen was recognized in 1941 and named “C” because it was the next available letter in the alphabet after A and B antigen nomenclature. The antibody is IgM and IgG and can cause a mild to severe, immediate/delayed transfusion reaction. Anti-C can also cause mild hemolytic disease of the fetus and newborn (HDFN). The optimal technique for detection is the indirect antiglobulin test (IAT).IncorrectThe patient’s serum on panel 1 showed she is group A-, with anti-D and anti-C.
Anti-D Discussion
After the ABO system, the Rh system is the most important blood group system in transfusion medicine with D being the most immunogenic Rh antigen. The original ‘Rh’ antigen stimulated a transfusion reaction, which was investigated by Levine and Stetson in 1939. The reactions of this antibody paralleled those of the anti-’Rh’ reported by Landsteiner and Wiener in 1940 but stimulated in animals. Years later, upon recognition that the human and the animal anti-’Rh’ did not react with the same antigen, the antigen name switched to D and the system took the Rh name. Testing for the D antigen is included as part of routine donor and patient typing with “Rh positive” and “Rh negative” referring to the presence or absence of the D antigen on red blood cells. The D antigen is distinguished from other blood group antigens in that it is composed of at least 30 epitopes distributed along the extracellular portions of the RhD protein.
Most anti-D is IgG with some IgM and can cause a mild to severe, immediate/delayed transfusion reaction. Anti-D can also cause mild to severe hemolytic disease of the fetus and newborn (HDFN). The optimal technique for detection is the indirect antiglobulin test (IAT). Saline IAT is used in this case to identify IgM anti-D, confirming , rule out Rh-Ig.Anti-C Discussion
The C antigen was recognized in 1941 and named “C” because it was the next available letter in the alphabet after A and B antigen nomenclature. The antibody is IgM and IgG and can cause a mild to severe, immediate/delayed transfusion reaction. Anti-C can also cause mild hemolytic disease of the fetus and newborn (HDFN). The optimal technique for detection is the indirect antiglobulin test (IAT). -
Question 2 of 3
2. Question
What are the possible RH genotypes of the mother?
CorrectAlthough there have been rare reports of D positive, G negative individuals typically, the only phenotypes that would result in G negative red blood cells are rr (dce/dce), rr”" (dce/dcE), and r”"r”" (dcE/dcE). As a result, most individuals are G positive. The rr phenotype is the most common and occurs in approximately 15% of the US population while rr” and r”r” occur in
IncorrectAlthough there have been rare reports of D positive, G negative individuals typically, the only phenotypes that would result in G negative red blood cells are rr (dce/dce), rr”" (dce/dcE), and r”"r”" (dcE/dcE). As a result, most individuals are G positive. The rr phenotype is the most common and occurs in approximately 15% of the US population while rr” and r”r” occur in
-
Question 3 of 3
3. Question
What underlying antibody you should also consider? How do you work it up?
CorrectAnti-G Abs
The G antigen was first described in 1958 by Allen and Tippett as an antigen distinct from C and D. The initial investigation also showed that most serums containing “anti-CD” actually contained anti-G. Present on nearly all red cells that demonstrate either the D or C antigen; the G antigen is usually absent only when a person’s red cells lack both the D and C antigen.
Patient should be followed up for anti-D and C titer. Anti-G antibody should be worked up using double absorption technique. In addition, father’s RBC phenotyping, mother’s RBC phenotype and genotyping can be carried out. Fetus should be closely monitored for hemolytic disease of the fetus.IncorrectAnti-G Abs
The G antigen was first described in 1958 by Allen and Tippett as an antigen distinct from C and D. The initial investigation also showed that most serums containing “anti-CD” actually contained anti-G. Present on nearly all red cells that demonstrate either the D or C antigen; the G antigen is usually absent only when a person’s red cells lack both the D and C antigen.
Patient should be followed up for anti-D and C titer. Anti-G antibody should be worked up using double absorption technique. In addition, father’s RBC phenotyping, mother’s RBC phenotype and genotyping can be carried out. Fetus should be closely monitored for hemolytic disease of the fetus.
CLINICAL HISTORY – Part II
In the course of this pregnancy, anti-D titer, rose from 64 (week 20) to 128 (week 24), then to1024 (week 28) and remained at 1024 at the final analysis in week 37. Anti-C identified with titer 8 (week 20) and remained discrete at 1 in gestation weeks 24 and 1 in week 28.
The aliquote of mother’s plasma was adsorbed three times with papain treated D-C+G+ RBCs after which anti-D was detected by Saline IAT.
An aliquot of the patient’s plasma was adsorbed onto either D-C+G+ and D+C-G+ RBCs, and acid elutes were prepared from both aliquots of sensitized RBCs (Table 2).
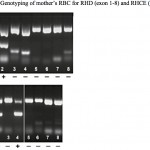
Genotyping of mother’s RBC for RHD (exon 1-8) and RHCE (exon 1-8) was also performed (Figure 1).
Multiple intrauterine transfusion were conducted and the mother delivered at 36 weeks.
Quiz-summary
0 of 2 questions completed
Questions:
- 1
- 2
Information
BEGIN QUIZ 2/2:
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading...
You must sign in or sign up to start the quiz.
You have to finish following quiz, to start this quiz:
Results
0 of 2 questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 points, (0)
| Average score |
|
| Your score |
|
Categories
- Not categorized 0%
-
Click ‘VIEW QUESTIONS‘ for the discussion.
- 1
- 2
- Answered
- Review
-
Question 1 of 2
1. Question
Should the mother receive Rh-Ig?
CorrectIt is important to differentiate between anti-D plus anti-C and anti-G in prenatal evaluations as anti-G has been associated with hemolytic disease of the fetus and newborn (HDFN). It is also very important to distinguish anti-D plus anti-C and anti-G in OB patients to determine if the patient should receive RhIg. If the antibody is anti-D, the patient does not require RhIg; if the antibody is anti-G, RhIg administration would be recommended to prevent the formation of anti-D.
Anti-D and anti-C are frequent antibodies. Studies showed anti-D accounted for 46% of all pregnancy-related antibodies and anti-C for no more than 1%. Both are known to cause severe HDN. Since both antibodies often occur in combination, identification of an anti-G that comprises both epitopes on the D and C antigen is often unrecognized. Even combinations of anti-C and anti-G, in the absence of anti-D, are found to cause severe HDN. However, little data exists on the presence of anti-G on its own during pregnancies. This antibody is rarely diagnosed and may occur more often in pregnancies due to the high frequency of C and D in the population. However, women that present anti-G antibodies can develop additional anti-D. An accurate differentiation between anti-C plus anti-D and anti-G is of high importance in pregnancies. When anti-D is absent, rhesus prophylaxis must be administered.IncorrectIt is important to differentiate between anti-D plus anti-C and anti-G in prenatal evaluations as anti-G has been associated with hemolytic disease of the fetus and newborn (HDFN). It is also very important to distinguish anti-D plus anti-C and anti-G in OB patients to determine if the patient should receive RhIg. If the antibody is anti-D, the patient does not require RhIg; if the antibody is anti-G, RhIg administration would be recommended to prevent the formation of anti-D.
Anti-D and anti-C are frequent antibodies. Studies showed anti-D accounted for 46% of all pregnancy-related antibodies and anti-C for no more than 1%. Both are known to cause severe HDN. Since both antibodies often occur in combination, identification of an anti-G that comprises both epitopes on the D and C antigen is often unrecognized. Even combinations of anti-C and anti-G, in the absence of anti-D, are found to cause severe HDN. However, little data exists on the presence of anti-G on its own during pregnancies. This antibody is rarely diagnosed and may occur more often in pregnancies due to the high frequency of C and D in the population. However, women that present anti-G antibodies can develop additional anti-D. An accurate differentiation between anti-C plus anti-D and anti-G is of high importance in pregnancies. When anti-D is absent, rhesus prophylaxis must be administered. -
Question 2 of 2
2. Question
If panel 1 (table 1) result is obtained from a 50 year old male patient during pre-transfusion test, will your strategy be different?
CorrectSince anti-G looks like a combination of anti-D and anti-C, it can be quite confusing when seen in an Rh negative patient who has no history of being exposed to D positive blood. For pretransfusion testing, it is not important to differentiate anti-G from anti-D plus anti-C. In either instance, the patient would be transfused with D negative blood, and since the vast majority of Rh negative blood has the rr phenotype, these units would most likely be G negative and crossmatch compatible.
IncorrectSince anti-G looks like a combination of anti-D and anti-C, it can be quite confusing when seen in an Rh negative patient who has no history of being exposed to D positive blood. For pretransfusion testing, it is not important to differentiate anti-G from anti-D plus anti-C. In either instance, the patient would be transfused with D negative blood, and since the vast majority of Rh negative blood has the rr phenotype, these units would most likely be G negative and crossmatch compatible.
TABLES/FIGURES
Presented by : Drs. Wendi Zhou and Mark T. Friedman